| Category | Nerve Blocks |
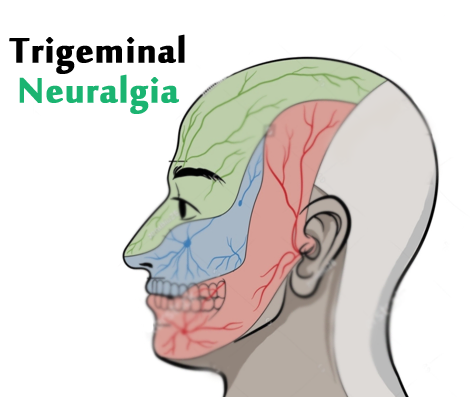
It is a condition characterized by pain coming from the trigeminal nerve, which starts near the top of the ear and splits in three, toward the eye, cheek and jaw. We have two trigeminal nerves for each side of our face, but trigeminal neuralgia pain most commonly affects only one side.
The pain of trigeminal neuralgia is unlike facial pain caused by other problems. It is often described as stabbing, lancinating or electrical in sensation and so severe that the affected person cannot eat or drink. The pain travels through the face in a matter of seconds, but as the condition progresses, the pain can last minutes and even longer.
Trigeminal neuralgia is sometimes known as tic douloureux, which means "painful tic."
Trigeminal neuralgia usually occurs spontaneously, but is sometimes associated with facial trauma or dental procedures.
The condition may be caused by a blood vessel pressing against the trigeminal nerve, also known as vascular compression. Over time, the pulse of an artery rubbing against the nerve can wear away the insulation, which is called myelin, leaving the nerve exposed and highly sensitive.
The resulting symptoms can be similar to those caused by dental problems, and sometimes people with undiagnosed trigeminal neuralgia explore multiple dental procedures in an effort to control the pain.
Multiple sclerosis or a tumor can also cause trigeminal neuralgia.
Trigeminal neuralgia occurs more often in women than men, is more common in older people (usually 50 and older), and occurs more on the right than the left. It doesn’t usually run in families.
Clinical testing and imaging or laboratory tests, high-resolution MRI of the trigeminal nerve and surrounding areas. These tests can help determine if the pain is caused by a tumor or blood vessel abnormality, or by undiagnosed multiple sclerosis. Certain advanced MRI techniques may help to see where a blood vessel is pressing against a branch of the trigeminal nerve.
Medications
Many people who suffer from trigeminal neuralgia successfully manage this condition for many years with medication. Regular blood tests may be required for some medications to check your white blood cell count, platelets, sodium levels and liver function.
Your neurologist or primary care physician can help you select the best drug and the most appropriate dosage. Most patients start out on low doses, gradually increasing the dose under clinical supervision until they achieve the best pain relief with the least amount of side effects.
Nerve blocks are injections (with a steroid medication or another agent) made at various parts of the nerve to reduce pain. They may provide pain relief for people with trigeminal neuralgia.
The use of high-resolution ultrasound facilitates real-time visualization of peripheral nerves and adjacent soft tissue structures, such as tendons, ligaments, muscles, vessels, and subcutaneous fat.
Ultrasound-guided intervention allows precise targeting of the affected nerves without collateral damage to the nearby vessels and prevents accidental nerve injury, vascular thrombosis, and post injection hematoma

Patients with TN who have good to excellent pain relief with a diagnostic trigeminal ganglion block may be suitable candidates for percutaneous RF rhizotomy, especially if the pain relief is of a short duration. It is performed by destruction of the trigeminal ganglion or roots using RF.
RF is the most common percutaneous procedure used to treat TN, especially in elderly patients.The procedure is performed under fluoroscopic guidance with the patient in the supine position and head extended.
After percutaneous RF rhizotomy, initial pain relief can be achieved in 98% of patients. Although 15%–20% of patients may experience recurrence pain in 12 months, recurrence rate is the lowest among all the percutaneous techniques.
The doctor will clean the area over the region of interest and insert a small needle into the target area under imaging guidance. When it is in the correct position, they will inject the drug. They will remove the needle and cover the injection site with a small dressing.
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is few hours
Every procedure carries a risk, although this is extremely small. The risk of infection with this procedure is extremely small as no incisions are made in the skin.
You can resume your work after 1 day if existing disease allows.