| Category | Spinal (Back Pain) |
Of all the patients who are dealing with low back pain, in approximately 30-40% of these cases, pain is caused by a discogenic cause.
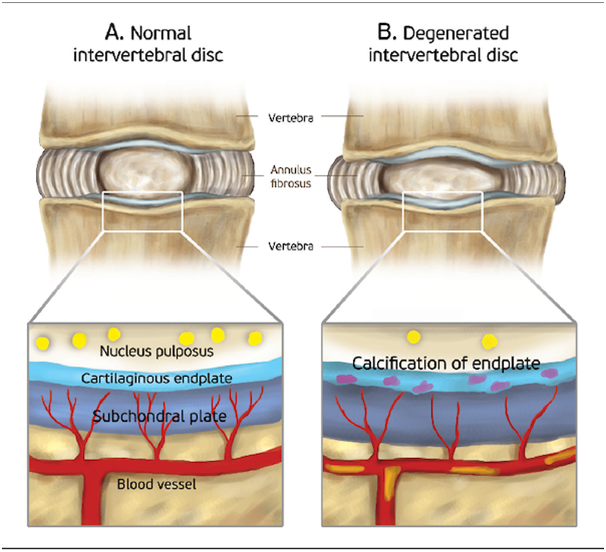
Discogenic pain is pain originating from a damaged vertebral disc, particularly due to degenerative disc disease. Disc degeneration occurs naturally with age.
The intervertebral discs have 2 parts: the inner nucleus pulposus and the outer annulus fibrosus. The inner part (nucleus pulposus) has no nerve supply. But the nerve supply of the outer third of the annulus fibrosus makes it susceptible to pain upon any damage to it. Due to the process of degeneration, cracks appear in the outer part. The gelatinous material of the nucleus pulposus enters these cracks. The degenerating disc also releases many pain-causing substances in addition to growth factors that result in nerve growth into the disc.
Pain increases with activities that increase pressure on the discs, such as sitting, bending, twisting, lifting, coughing, and sneezing. The patient decreases by changing position or walking.
Other symptoms include tenderness, back weakness, muscle spasms, and the feeling of back instability.
We will make the diagnosis of lumbar discogenic back pain based on a combination of the following:
Medical history of your activities such as excessive driving, lifting heavy objects, bending for excessive periods, tobacco smoking, etc.
Physical examination to check for tenderness, numbness, and the range of back motion. We will observe your gait and ask you to bend or twist your back to check for the range of back motion.
X-rays don’t help diagnose lumbar discogenic back pain but help rule out other spine-related conditions.
MRI can make a diagnosis. These tests can clearly show the degeneration of intervertebral discs and damage to other soft tissues.
There is no permanent cure for degenerating intervertebral discs. The goal of treatment is to manage symptoms and slow disease progression.
Rest and reducing or modifying activities that aggravate the pain
Pain killers and muscle relaxants
Physical therapy consisting of stretching exercises, strengthening exercises, and low-impact aerobic exercises is recommended. These are to relieve pressure on the back and build a healthy posture of the back.
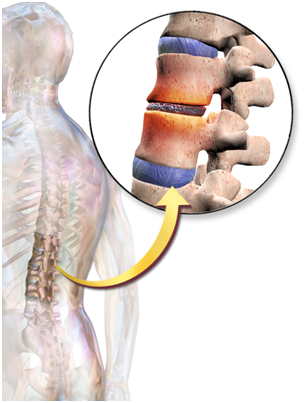
Your spinal column is made up of a series of bones (vertebrae) stacked onto each other. From top to bottom, the column includes seven bones in the cervical spine, 12 in the thoracic spine, and five in the lumbar spine, followed by the sacrum and the coccyx at the base. These bones are cushioned by discs. The discs protect the bones by absorbing the shocks from daily activities like walking, lifting, and twisting.
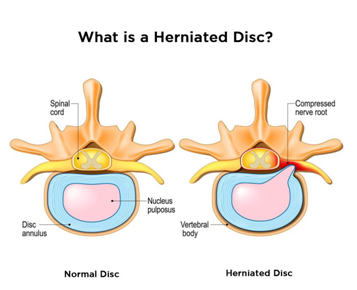
Each disc has two parts: a soft, gelatinous inner portion and a tough outer ring. Injury or weakness can cause the inner portion of the disc to protrude through the outer ring. This is known as a slipped, herniated, or prolapsed disc. This causes pain and discomfort. If the slipped disc compresses one of your spinal nerves, you may also experience numbness and pain along the affected nerve. In severe instances, you may require surgery to remove or repair the slipped disc.
You can have a slipped disc in any part of your spine, from your neck to your lower back. The lower back is one of the more common areas for slipped discs. Your spinal column is an intricate network of nerves and blood vessels. A slipped disc can place extra pressure on the nerves and muscles around it.
A slipped disc occurs when the outer ring becomes weak or torn and allows the inner portion to slip out. This can happen with age. Certain motions may also cause a slipped disc. A disc can slip out of place while you are twisting or turning to lift an object. Lifting a very large, heavy object can place great strain on the lower back, resulting in a slipped disc. If you have a very physically demanding job that requires a lot of lifting, you may be at increased risk for slipped discs.
Overweight individuals are also at increased risk for a slipped disc because their discs must support the additional weight. Weak muscles and a sedentary lifestyle may also contribute to the development of a slipped disc.
As you get older, you are more likely to experience a slipped disc. This is because your discs begin to lose some of their protective water content as you age. As a result, they can slip more easily out of place. They are more common in men than women.

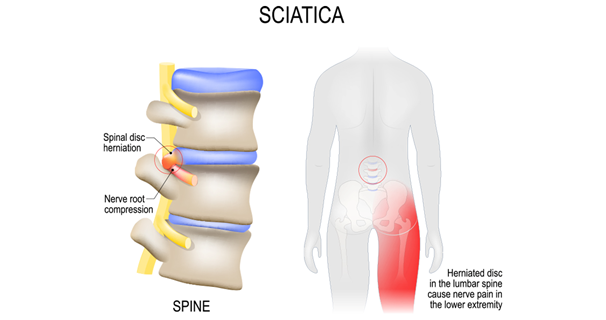
An untreated, severe slipped disc can lead to permanent nerve damage. In very rare cases, a slipped disc can cut off nerve impulses to the cauda equina nerves in your lower back and legs. If this occurs, you may lose bowel or bladder control.
Another long-term complication is known as saddle anesthesia. In this case, the slipped disc compresses nerves and causes you to lose sensation in your inner thighs, the back of your legs, and around your rectum.
While the symptoms of a slipped disc may improve, they also can worsen. If you cannot perform the activities you once could, it’s time to see your doctor.
We will look for the source of your pain and discomfort. This will involve checking your nerve function and muscle strength, and whether you feel pain when moving or touching the affected area. We also will ask you about your medical history and your symptoms.
Imaging tests can help view the bones and muscles of your spine and identify any damaged areas. Examples of imaging scans include:
We can combine all these pieces of information to determine what is causing your pain, weakness, or discomfort.

Range from conservative to surgical. The treatment typically depends on the level of discomfort you’re experiencing and how far the disc has slipped out of place.
Few people can relieve slipped disc pain using an exercise program that stretches and strengthens the back and surrounding muscles. A physical therapist may recommend exercises that can strengthen your back while reducing your pain.
Taking over-the-counter pain relievers and avoiding heavy lifting and painful positions can also help.
While it may be tempting to refrain from all physical activity while you’re experiencing the pain or discomfort of a slipped disc, this can lead to muscle weakness and joint stiffness. Instead, try to remain as active as possible through stretching or low-impact activities such as walking.
If your slipped disc pain does not respond to over-the-counter treatments, minimally invasive treatments can help you in order to increase cost-effectiveness and reduce long-term side effects. These include:
Epidural or Foraminal steroid injection. An injection of a cortisone-like medicine into the space around the nerve may provide pain relief by reducing inflammation.
There is good evidence that epidural injections can successfully relieve pain in many patients who have not been helped by medicines
It is important to note that these nonsurgical treatments do not heal the herniated disk. Rather, they can help relieve your symptoms while your body works to heal the disk. In many cases, the disk herniation naturally dissolves over time and is reabsorbed by the body.
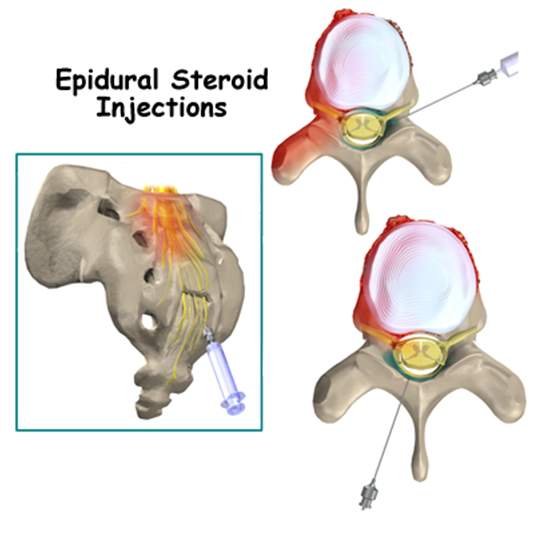
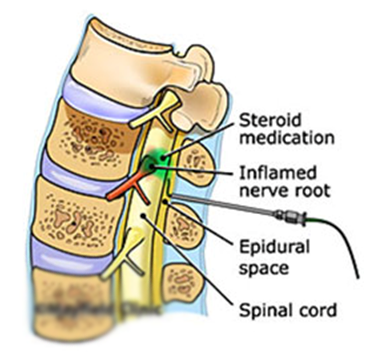
The doctor will clean the area over the spine and insert a small needle into the target area under imaging guidance. When it is in the correct position, they will inject the drug. They will remove the needle and cover the injection site with a small dressing.
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around few hours.
Every procedure carries a risk, although this is extremely small. The risk of infection with this procedure is extremely small as no incisions are made in the skin.
You can resume your work after 1 day if existing disease allows.
These are minimally invasive therapy used for treatment of disk herniations. Percutaneous removal of nucleus pulposus has been performed with a variety of chemical and mechanical techniques. These techniques consist of removing all or part of the nucleus pulposus to induce more rapid healing of the pathological lumbar disk. Percutaneous nucleotomy is now widely used, as it is much less invasive than surgical discectomy.
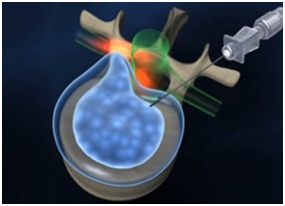
Percutaneous laser disk decompression (PLDD), and nucleoplasty (radiofrequency disk decompression) have the same goal through slightly different means and are designed to remove the center of the disk.
Last resort is Surgery- Microdiskectomy or in more severe cases, your doctor may replace the disc with an artificial one or remove the disc and fuse your vertebrae together.
The doctor will clean the area over the spine and insert a small needle into the target area under imaging guidance. When it is in the correct position, they will perform the procedure. They will remove the needle and cover the injection site with a small dressing.
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around few hours.
Every procedure carries a risk, although this is extremely small. The risk of infection with this procedure is extremely small as no incisions are made in the skin.
You can resume your work after 1 day if existing disease allows.